Spectral Medicine: Uncovering how different wavelengths of light revolutionize modern medicine
From ultraviolet sterilization to infrared repair, a therapeutic revolution written by photons is quietly happening in hospitals around the world.
When the ancient Egyptians first consciously used sunlight to treat diseases, they would not have thought that thousands of years later, doctors are manipulating a light wave arsenal accurate to nanometers** to fight diseases – 311nm ultraviolet rays accurately snipe psoriasis plaques, 808nm infrared lasers penetrate deep into joints to reduce inflammation, and 633nm red light accelerates the healing of diabetic ulcers.
The medical application of light has surpassed simple thermal effects and sterilization and entered an era of precision with wavelength specificity and cell pathway targeting. Under the surface of the skin, photons of different wavelengths are like agents with different keys, accurately unlocking mitochondria, pigment groups or DNA repair mechanisms in cells, and starting the body’s own treatment program.
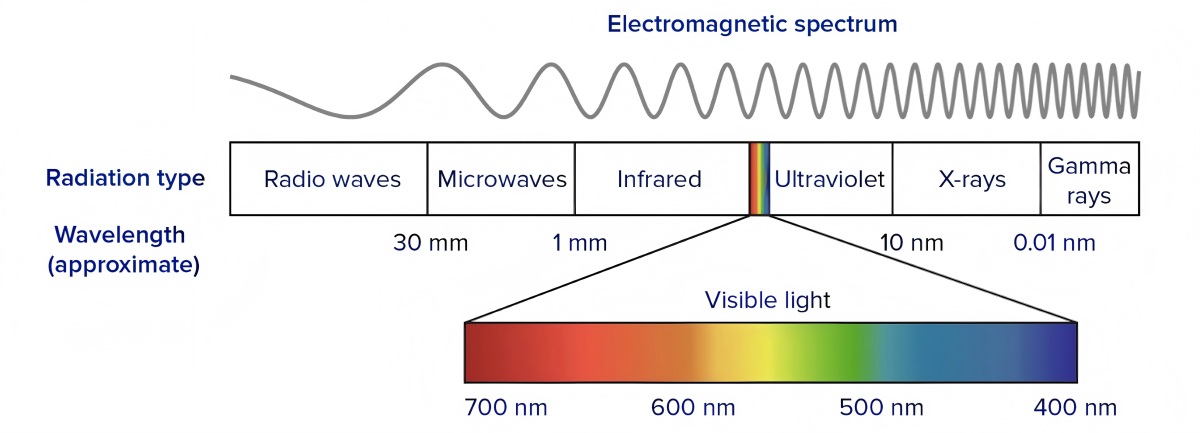
1 Wavelength penetration map, the basic law of optical medicine
The medical application of light is first a competition of penetration depth. There are significant differences in the ability of photons of different wavelengths to penetrate human tissue, and this characteristic directly determines their medical application scenarios.
Ultraviolet light (100-400nm) is at the short-wave end of the spectrum, among which UVB (290-320nm) mainly acts on the epidermis, and has been proven to effectively inhibit the excessive proliferation of keratinocytes, becoming the gold standard for the treatment of psoriasis. UVA (320-400nm) can reach the superficial dermis with its longer wavelength, activating photosensitizers in deep lesions in photodynamic therapy.
The penetration of visible light (400-760nm) presents a color gradient change. Blue light (440-500nm) stays in the upper layer of the epidermis, but its antibacterial properties make it a powerful tool for acne treatment; red light (620-750nm) can penetrate deep into the dermis and even subcutaneous tissue to promote deep wound repair.
In the infrared light family, near-infrared light (700-1400nm) has become a true “deep penetrator” that can reach muscles, nerves and bones, providing the possibility for deep tissue repair and nerve regulation. This “matching game” between wavelength and tissue is the basis for the precision of optical medicine.
2 The double-edged sword of ultraviolet light, the precise balance between treatment and risk
The application of ultraviolet medical treatment shows the scientific wisdom of how humans transform a carcinogenic factor into a therapeutic tool. As a pillar of modern dermatology, narrow-spectrum UVB (311-313nm) can treat psoriasis with an effective rate of more than 75% by inducing T cell apoptosis and inhibiting abnormal proliferation of epidermal cells.
The 308nm excimer laser pushes this precision to a new level, and its spot can accurately cover the vitiligo lesion area, minimizing the exposure of surrounding normal tissues. In the field of photodynamic therapy (PDT), the combination of UVA and photosensitizers creates an “optical scalpel” for cancer treatment.
When topical aminolevulinic acid (ALA) is enriched in cancerous tissue, UVA irradiation produces singlet oxygen, selectively destroying basal cell carcinoma cells, with a cure rate of 93%. This “molecular targeting” property makes PDT particularly suitable for the treatment of cosmetically sensitive areas such as the face.
The core challenge of ultraviolet medical treatment lies in risk control. Professional equipment reduces the risk of cancer to an acceptable level through dose algorithms and irradiation range control, while the benefits of treatment significantly exceed the risks.
3 The multi-color revolution of visible light, from jaundice treatment to neuromodulation
The medical application of the visible spectrum is like a color revolution. The treatment of neonatal jaundice with blue light (around 460nm) is the most classic application. Through photoisomerization, toxic fat-soluble bilirubin is converted into water-soluble isomers to avoid brain damage caused by kernicterus.
In dermatology, the antibacterial properties of blue light are used to remove Propionibacterium acnes, while red light promotes fibroblast proliferation and collagen synthesis, accelerating chronic wound healing.
The most groundbreaking progress in recent years comes from the neuromodulatory function of near-infrared light (although invisible, it is often used in combination with visible red light). Near-infrared photobiomodulation (PBM) can penetrate the skull and act on the mitochondria of the cerebral cortex.
Cytochrome C oxidase absorbs photons and increases ATP production by 40-50%, improving nerve cell metabolism. Clinical studies have confirmed that transcranial near-infrared light therapy can significantly improve the cognitive function of patients with traumatic brain injury and the memory test scores of patients with Alzheimer’s disease, providing a new non-drug intervention option for neurodegenerative diseases.
4 Deep treatment of infrared light, from wound repair to anti-inflammatory mechanism
Infrared light, especially the near-infrared band (700-1100nm), is in the midst of an explosion of medical applications, thanks to its excellent tissue penetration ability and unique photobiomodulatory effect.
In the field of tissue repair, near-infrared light has been shown to accelerate the healing of diabetic foot ulcers. A randomized controlled trial showed that after 8 weeks of combined use of 625, 660 and 850nm light (2.4J/cm²) 3 times a week, the wound area in the treatment group was significantly smaller than that in the control group.
Mechanism studies have found that near-infrared light continuously affects cell function through epigenetic regulation. After mitochondria absorb near-infrared photons, they activate histone modification enzymes, turn on the anti-inflammatory gene expression switch, and transform macrophages from pro-inflammatory M1 to reparative M2.
This effect is manifested in animal experiments as increased TGF-β1 secretion and decreased TNF-α levels, providing a scientific basis for near-infrared light treatment of chronic inflammatory diseases such as rheumatoid arthritis.
Tissue penetration depth and therapeutic applications of light of different wavelengths
| Wavelength type | Wavelength range (nm) | Penetration depth | Main medical applications | |
|---|---|---|---|---|
| UVB | 290-320 | Epidermis | Psoriasis, vitiligo treatment | |
| UVA | 320-400 | Superfic20-400 | Superficial dermis | Photodynamic therapy, scleroderma treatment |
| Blue light | 440-500 | Epidermis | Neonatal jaund Epidermis | Neonatal jaundice, acne treatment |
| Red light | 620-750 | Dermis-subcutaneous | Wound healing, anti-inflammatory treatment | |
| Near infrared light | 700-1400 | Muscle/nerve | Deep tissue repair, neuromodulation |
5 Photobiomodulation, the medical transformation of cellular energetics
Photobiomodulation (PBM) represents a paradigm shift in optical medicine from thermal effects to biomodulation. This technology uses low-energy light sources (1-5W/cm²) to activate endogenous chromophores. The core mechanism lies in precise regulation of mitochondrial energetics.
Cytochrome c oxidase (CCO), as the main photoreceptor, undergoes conformational changes after absorbing 630-670nm red light or 780-940nm near-infrared light, dissociates inhibitory nitric oxide, improves respiratory chain efficiency, and increases ATP production by 50-70%.
This improvement in bioenergetics triggers a cascade effect: the increase in cyclic adenosine monophosphate (cAMP) levels activates the protein kinase A pathway; reactive oxygen species (ROS) act as signal molecules to activate transcription factors such as nuclear factor κB, regulating more than 200 gene expressions.
In clinical transformation, the bidirectional dose effect of PBM follows the Arndt-Schulz law: too low energy is ineffective, moderate energy (1-10J/cm²) stimulates, and too high energy inhibits. This nonlinear relationship requires that the treatment parameters must be precisely calibrated.
Currently, PBM has achieved the most significant success in the field of wound repair, shortening the healing time of chronic ulcers by 30-50% by promoting fibroblast proliferation, orderly collagen deposition and angiogenesis.
6 Multi-wavelength synergy and the future, a new era of integrated laser medical treatment
The next frontier of optical medicine is multi-wavelength synergistic treatment and localization of high-end equipment. The thulium-holmium dual-wavelength laser therapy machine developed in China (thulium laser: 1850-2050nm; holmium laser: 2100nm) has made a breakthrough in solving the clinical pain points of urology.
Traditionally, prostate hyperplasia requires fine cutting with thulium laser, while bladder stones require lithotripsy with holmium laser. The dual-wavelength system integrates two lasers into a single device through an intelligent control system and fiber coupling technology, and outputs them through the same fiber, shortening the operation time by 40% and avoiding the risk of infection during equipment replacement.
This “two-in-one” design concept represents the future direction – improving treatment efficiency through wavelength complementarity. At the industrial level, although China’s medical lasers have made significant progress, core components such as ultrafast lasers used for precision diagnosis and treatment still rely on imports.
Strategic research recommends the establishment of a secondary discipline of laser medicine, the construction of a national research and development platform, focusing on the “bottleneck” technology of medical lasers, and promoting the localization of high-end equipment.
Clinical application and effect of photobiomodulation (PBM)
| Disease area | Mechanism of action | Clinical effect | Recommended wavelength and energy density |
|---|---|---|---|
| Diabetic foot ulcer | Promote angiogenesis and enhance collagen synthesis | Wound area reduced by more than 60% after 8 weeks of treatment | 660nm+850nm, 2.4J/cm² |
| Neurodegenerative diseases | Increase mitochondrial ATP production in neurons | Cognitive function score improved by 30-40% | 810nm, 6J/cm² |
| Arthritis | Inhibit proinflammatory factors and promote M2 macrophage polarization | Pain score reduced by 50%, joint range of motion improved | 980nm, 3J/cm² |
| Refractory wounds | Promote fibroblast proliferation and migration | Healing time shortened by 30-50% | 633nm, 4J/cm² |
The future of laser medicine is emerging in integration and intelligence. The multiphoton imaging system developed by the team of Huazhong University of Science and Technology has achieved real-time brain tumor identification during surgery, and optical technology is breaking the boundaries between diagnosis and treatment.
From ultraviolet light therapy to near-infrared neuromodulation, from single-wavelength devices to thulium-holmium dual laser systems, humans have mastered the key of photons to unlock the therapeutic code in cells. When light of different wavelengths travels deep into human tissue like precise medical missiles, modern medicine is writing a therapeutic revolution encoded by light.
And the core rules of this revolution have never changed: specific wavelength, precise targeting, minimum damage, maximum efficacy-the four golden laws of light wave medicine are reshaping the future form of medical care.
FAQ:
Q1: How does light therapy work medically?
A: Specific wavelengths trigger cellular mechanisms (e.g., mitochondrial activation, DNA repair).
Q2: Which light treats psoriasis?
A: Narrow-band UVB (311nm) targets overactive skin cells.
Q3: Can light penetrate deep tissues?
A: Near-infrared (700-1400nm) reaches muscles/nerves for inflammation reduction.
Q4: Is light therapy safe?
A: Controlled-dose UV therapy minimizes cancer risk while maximizing benefits.
Q5: What’s photobiomodulation (PBM)?
A: Low-energy light (e.g., 660nm) boosting ATP production for wound healing.
Q6: Which light helps brain disorders?
A: 810nm near-infrared improves cognitive function in Alzheimer’s patients.
